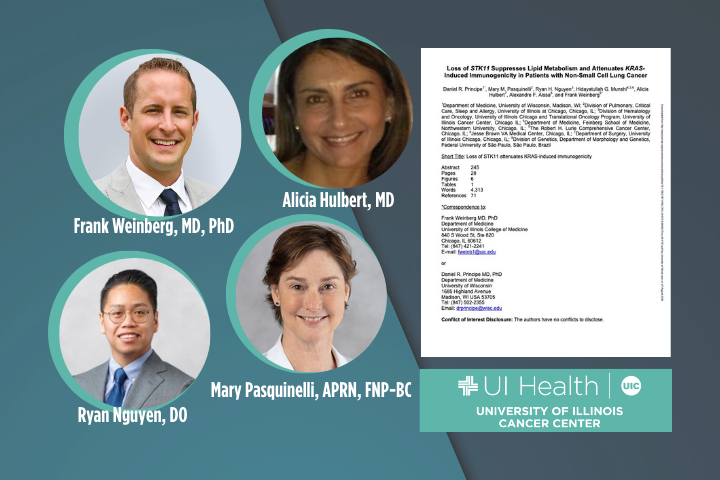
University of Illinois Cancer Center member and UI Health oncologist Frank Weinberg, MD, PhD, is a corresponding author on a new study that investigated the underlying mechanisms of immunotherapy resistance in specific types of KRAS-mutated lung cancer and used samples from UI Health patients with non-small cell lung cancer.
Published in Cancer Research Communications, a journal of the American Association for Cancer Research, the study included other Cancer Center member, UI Health and University of Illinois Chicago (UIC) authors: Ryan Nguyen, DO, Mary Pasquinelli, APRN, FNP-BC and Alicia Hulbert, MD, as well as authors from other institutions.
The abstract from the study, “Loss of STK11 Suppresses Lipid Metabolism and Attenuates KRAS-Induced Immunogenicity in Patients with Non-Small Cell Lung Cancer,” is excerpted below.
“As many as 30% of non-small cell lung cancer (NSCLC) patients harbor oncogenic KRAS mutations, which lead to extensive remodeling of the tumor immune microenvironment. Though co-mutations in several genes have prognostic relevance in KRAS-mutated patients, their effect on tumor immunogenicity are poorly understood. In the present study, a total of 189 NSCLC patients underwent a standardized analysis including immunohistochemistry, whole exome DNA sequencing, and whole transcriptome RNA sequencing. Patients with activating KRAS mutations demonstrated a significant increase in PD-L1 expression and CD8+ T-cell infiltration. Both were increased in the presence of a co-occurring TP53 mutation and lost with STK11 co-mutation. Subsequent genomic analysis demonstrated that KRAS/TP53 co-mutated tumors had a significant decrease in the expression of glycolysis-associated genes, and increase in several genes involved in lipid metabolism, notably Lipoprotein Lipase (LPL), Low Density Lipoprotein Receptor (LDLR), and LDLRAD4. Conversely, in the immune-excluded KRAS/STK11 co-mutated group, we observed diminished lipid metabolism and no change in anaerobic glycolysis. Interestingly, in patients with low expression of LPL, LDLR, or LDLRAD4, KRAS mutations had no effect on tumor immunogenicity. However, in patients with robust expression of these genes, KRAS mutations were associated with increased immunogenicity and associated with improved overall survival. Our data further suggest that the loss of STK11 may function as a metabolic switch, suppressing lipid metabolism in favor of glycolysis, thereby negating KRAS-induced immunogenicity. Hence, this concept warrants continued exploration, both as a predictive biomarker and potential target for therapy in patients receiving ICI-based immunotherapy.”
